The Complete Guide To Strong Bones Over 60 [Part 1]
PART 1: WHAT YOU NEED TO KNOW TO GET STRONGER BONES
In early life, keeping our bones strong is something we don’t think too much about!
We know our bones keep us standing.
We know that we can break our bones.
We know it’s important to have strong bones.
But…… that’s all we usually know about our bones most of our life. They just do their thing in the background and we get on with it.
It’s not until later in life that most people start to think more about keeping their bones healthy. This is usually because there is more talk about the effects of weaker bones, or a fracture occurs somewhere in the body, or, after tests, a doctor brings the news that your bones are weaker (which can come as quite a shock).
If you’re reading this article, having strong bones has most probably become important to you. Maybe you’ve been diagnosed with osteopenia or osteoporosis; maybe you’ve had fractures yourself, or maybe you want to make sure you’re doing all that you can to keep your bones at their strongest, which everyone should be doing.
In this article, we are going to be covering everything you need to know for healthiest bones.
In Part 1, we’ll learn about bones and how they work because having a better understanding of your body helps you to be healthier.
We’ll discuss osteopenia and osteoporosis, what is happening in these conditions and why they occur.
We will go through the testing procedures for determining bone strength and how often you should be getting your bone strength tested. We’ll also discuss the factors that contribute to bone strength (which goes beyond bone density).
In Part 2, we will go through all treatment approaches for improving bone strength and preventing fractures, from habits to cut out to nutrition (including vitamins and minerals for bone strength).
And in Part 3, we will cover all about exercise techniques for stronger bones, including some exercise programs (which include videos) that you can do to help promote bone strength.
After reading this article, you’ll have everything you need to make a difference in your bone health.
So read through it all, make the changes required and you’re on your way to better bone health.
Now…. Let’s get into it.
WHAT WE’LL BE COVERING IN PART 1:
ALL ABOUT YOUR BONES & BONE LOSS
WHAT HAPPENS TO OUR BONES AS WE GET OLDER - WHY DO OUR BONES BECOME WEAKER
OSTEOPENIA vs OSTEOPOROSIS: WHAT CAN HAPPEN WHEN BONES BECOME WEAKER
ALL ABOUT BONES AND BONE LOSS
EASING YOUR FEARS AROUND ‘BRITTLE BONES’ AND FRACTURES
To find out the structures of your body that hold you up, help you to move and to go about your daily activities are failing, and potentially going to get progressively worse over time, can be quite unsettling to say the least.
To think that your bones are now what’s commonly described as ‘brittle’ would not give anyone confidence in going about their day in fear of breaking a bone.
There are also some frightening statistics about hip fractures and the outcomes if this was to happen over a certain age that you may have heard (I.E. requiring permanent nursing care or even death not long after the fracture).
It makes the thought of getting older and the possibility of this occurring a terrifying and somewhat helpless situation.
But let’s look at this all from a different view.
Firstly, (I want to get this out of the way first), in regards to those statistics following a hip fracture, those who die following a hip fracture are usually very frail with serious health conditions prior to the fracture. Full recoveries can be made.
Secondly, it’s important to know that bone health is graded from normal (healthy bone levels) to mild bone loss and to osteoporosis (which has graded levels also).
Whatever your bone health is at this current time, you can prevent bone loss and loss in bone strength and it is possible to get them stronger.
As with many factors that are typically put down to ageing like muscle loss and strength, decreased fitness, and poor balance, weaker bones are also NOT due to ageing alone.
Yes, your bones will not be like they were when you were younger, but there are many other factors that contribute to loss of bone strength beyond ageing that can be changed.
Thirdly, being diagnosed with osteoporosis does not mean you’re definitely going to get fractures. Although osteoporosis does increase fracture risk and fractures are common with osteoporosis, there are many who get diagnosed with this condition that do not get fractures.
And finally, falls, which can lead to fractures, can be prevented.
There are always things you can do to improve your bone health and your situation.
Let’s focus now on what can be done to improve bone health and decrease fracture risk, starting with learning about our bones.
ABOUT YOUR BONES
Throughout life, the bones of our body are constantly being broken down (by cells known as osteoclasts) and then built up with new bone (by cells known as osteoblasts).
This process is called bone remodelling and it ensures that your body is well-adjusted to the ever-changing mechanical forces placed on it.
Basically, your body is continuously doing renovations to make sure that the whole structure maintains its integrity for the demands of life.
As children, our bones go through rapid periods of growth in both size and density where more bone is added than being taken away.
This increase in bone size and density continues into our late twenties when our skeleton reaches full maturation, and we reach what’s known as peak bone mass.
From this point, although our skeletal structure has now reached full maturation, bone remodelling continues to take place (now at a slower rate, however, in comparison to childhood).
To put it simply, as long as your body continues to create good quality bone tissue at the same (or similar rate) as it resorbs the old bone, your skeletal system remains strong and healthy.
WHAT HAPPENS TO OUR BONES AS WE GET OLDER - WHY DO OUR BONES GET WEAKER
As our body ages, the rate at which the new bone replaces the old bone slows down.
In other words, the resorption exceeds the formation of new bone tissue, leading to less bone mass.
Additionally, there is deterioration in the structure of the newly laid bone leading to poorer bone quality. [1]
This decline in quantity (density) and quality commonly results in conditions such as osteopenia and osteoporosis, predisposing one to the risk of fractures.
However, as touched on earlier, age-related bone loss is a complex disorder that occurs due to numerous factors and not just ageing alone. These factors include genetics, hormonal changes, as well as biochemical, lifestyle and environmental factors. We will cover this more later in this article.
OSTEOPENIA vs OSTEOPOROSIS: WHAT CAN HAPPEN WHEN BONES BECOME WEAKER
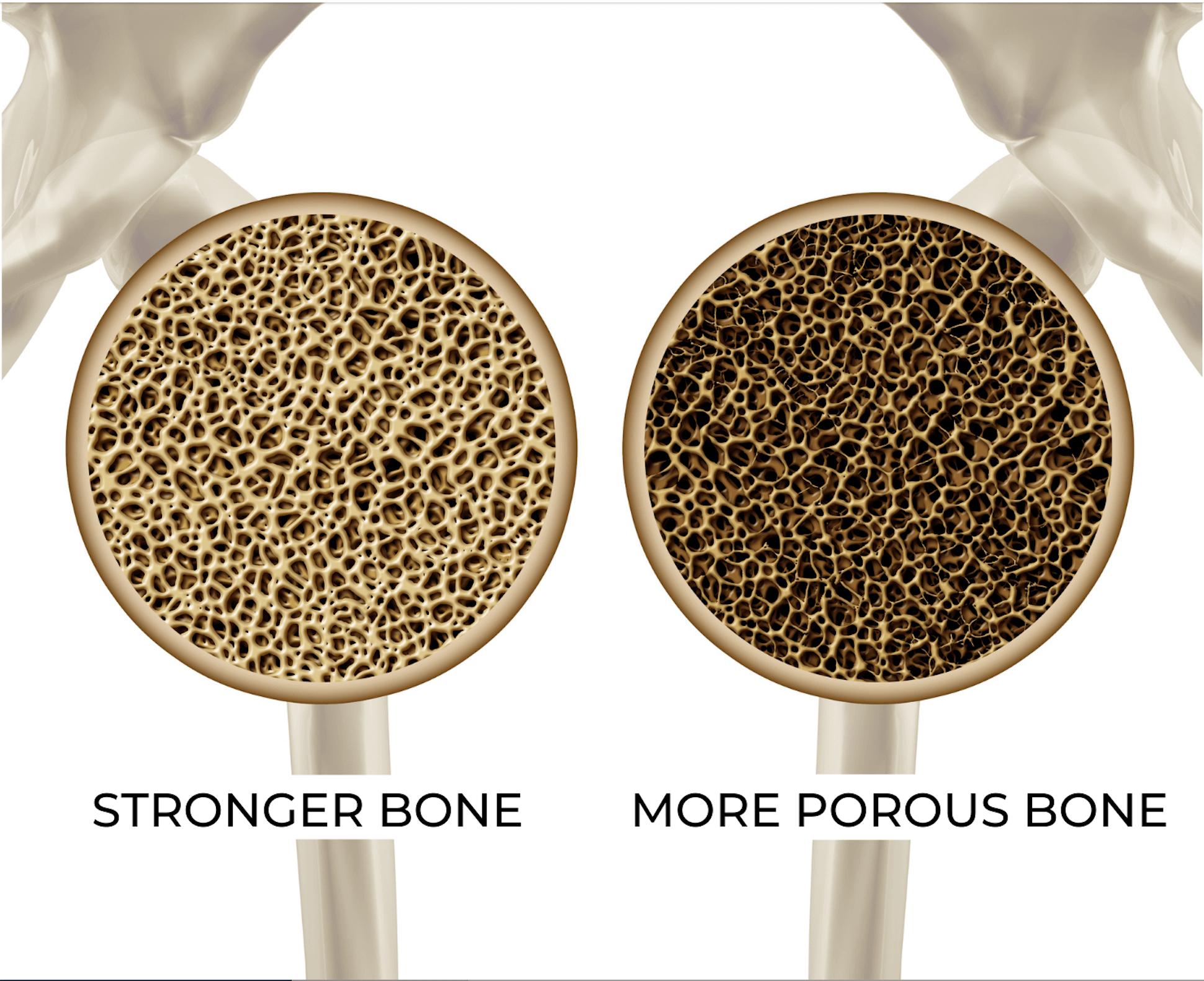
So when the rate of bone breakdown exceeds the rate of new bone formation, our bone mass decreases and becomes less dense (more porous).
When there is a loss in bone density, the first stage is what’s known as osteopenia.
If this loss in bone density was to progress further, we get into the ranges of osteoporosis.
Image: Healthy Hip Bone vs Porous Bone (Osteoporosis)
Osteoporosis is derived from Greek “osteon” (bone) and “poros” (little hole). Osteoporosis meaning ‘porous bone’. [2]
When bones become weaker, it can lead to secondary issues, the most common being fragility fractures.
As osteoporosis can affect any bone in the body, they are all at increased risk of fracture. However, fractures most commonly occur in bones that undertake more strain (such as the spine) or sites most at risk if one was to fall (wrists or hips).
Fractures can be painful and can lead to further problems, such as changes in posture, height loss, decreased quality of life, fear of further fractures, depression and social isolation.
HOW TO KNOW IF YOU HAVE BONE LOSS OR OSTEOPOROSIS
Osteoporosis can be present with no symptoms. Most of the time it usually goes undetected until a fracture occurs. For this reason, osteoporosis has been named the ‘silent disease’.
Osteoporosis can only be diagnosed by certain tests. If you are at risk of osteoporosis, your doctor will recommend and organise bone testing.
Let’s now look at the risk factors for osteoporosis.
RISK FACTORS FOR OSTEOPOROSIS
It’s important for you to be aware of the risk factors for bone loss and osteoporosis to know if you’re at risk and so you can get tested and take action if need be.
The following factors are risk factors for bone loss:
GENDER. Women are generally at higher risk of osteoporosis and osteopenia due to naturally having less bone mass than men.
Bone loss in women is most rapid following menopause with studies showing osteoporosis is related to estrogen deficiency.
By the age of 65-70, both men and women start losing bone at the same rate. [3]
AGE: Your risk for osteoporosis increases with age. Women over 65 and men over 70 are at greater risk.
BONE STRUCTURE & BODY WEIGHT: Thin people usually have a greater risk of developing osteoporosis due to having less bone mass to begin with. Additionally, those that have had major weight loss could also be at risk.
FAMILY HISTORY: Fracture risk secondary to osteoporosis is increased if a parent experiences a hip fracture, particularly if that fracture occurred at a younger age.
NUTRITION: Eating an inadequate amount of calories and consuming a poor diet limited, or devoid, of vital nutrients increases the risk of osteoporosis.
SEDENTARY LIFESTYLE: Lack of exercise and physical activity increases the risk of osteoporosis.
SMOKING AND EXCESSIVE ALCOHOL CONSUMPTION: Smoking decreases bone density and bone quality and increases the risk of fractures [4]. And the same goes for excessive alcohol consumption. [5]
HEALTH CONDITIONS: Certain conditions can put one at risk of developing osteoporosis. The diseases include thyroid disease or an overactive thyroid gland (hyperthyroidism), parathyroid disease or an overactive parathyroid (hyperparathyroidism), chronic kidney and liver disease, and rheumatoid arthritis, plus conditions that affect the body’s ability to absorb nutrients (e.g. Crohn’s disease, coeliac disease, and other inflammatory bowel conditions).
MEDICATIONS: Certain medications (e.g. corticosteroids or thyroid medications) can result in side effects that may damage bone and lead to osteoporosis.
Other possible signs of bone loss or osteoporosis:
Height Loss: 1/2 inch or more within one year. Or 1½ inches from your original height overall.
Past history of Fractures: - Fracture after age 50, fragility fracture at any age, or a spinal X-ray showing a fracture or bone loss in your spine
Pain: Back pain with potential spinal fracture
TESTING FOR BONE LOSS
HOW BONE LOSS IS COMMONLY TESTED
Firstly, a doctor will examine your medical history and ask questions to determine what risk factors (as discussed above) are present that could be putting you at risk of bone loss.
The doctor will also recommend a bone mineral density (BMD) test which is the primary and most commonly used test for bone loss.
Dual-energy X-ray absorptiometry (DEXA or DXA) is considered the gold standard for measuring bone mineral density.
Image: DEXA/DXA machine
The DEXA machine scans your body to measure bone mineral density at the hip and spine.
It measures the amount of minerals, namely calcium, in your bones and is a non-invasive and painless test that usually takes around 10 - 20 minutes.
Lab tests (blood and urine) may also be ordered which can help give more of a picture of what is going on with your bone health.
Lab tests can confirm or eliminate the existence of certain diseases or health problems that could contribute to bone loss or osteoporosis.
UNDERSTANDING BONE MINERAL DENSITY (DEXA) SCAN RESULTS
Once the DEXA scan is completed, the doctor will analyse the results using a T-score. A T-score compares a patient's bone density to the bone density of a healthy, young adult.
The bone density results are typically classified according to the following scores:
Normal Bone Density: between 1 and -1
Low Bone Density (Osteopenia): -1 to -2.5
Osteoporosis: -2.5 or lower
Severe Osteoporosis: -2.5 or lower with a history of bone fractures.
The DEXA test provides an important piece of information regarding your bone health. However, one DEXA scan can only give a snapshot of your bone at that point in time. It is not a definitive test to determine if you are losing bone.
IS BONE DENSITY THE ONLY FACTOR IN STRONG BONES?: INTRODUCING BONE QUALITY
Bone mineral density testing (DEXA) is the most widely used clinical tool by doctors to evaluate bone strength and risk of fracture due to its low radiation exposure and ease of use.
While this test is a considerably easy way to give an idea of bone strength and can help in making decisions for treatment and to determine treatment effectiveness, it is limited, however, to only measuring the mineral components of the bone, without any details regarding the structure of the bone.
This is important as bone density alone is not the only factor involved in bone strength and risk of fractures. Yes, lower bone density does correlate to increased fracture risk. [6, 7] However, bone density is only one component of bone strength. [8]
As discussed earlier in this article, as we get older we not only lose bone density (mass), we also get a change in the structure of the bone (or the quality).
A measurement of bone mineral density alone neglects other important contributors to bone strength and fracture risk reduction. Hence additional data is needed for predicting bone strength.
So…… What’s going on here?
As you’re starting to see, BONE DENSITY ALONE DOES NOT EQUAL BONE STRENGTH.
Bone strength is a combination of bone quantity (density and size) and bone quality, consisting of structure (micro and macro architecture), material properties, and bone turnover (remodelling). [9]
In simple terms, bone quality is related to what the bone is made up of and where this material is in regards to its structure, not just how dense the bone is, which is important to uphold the mechanical forces of the body.
BONE STRENGTH = BONE QUANTITY (DENSITY) + BONE QUALITY
This is important as the gold standard and most commonly utilised method for testing bone strength is bone mineral density. However, there is more evidence to show that bone quality is more important in predicting bone strength. [10]
HOW TO GET BONE QUALITY TESTED
At this point, you can see that bone density tests, the most commonly used test to determine bone strength, do not give a complete picture of your overall bone health.
You’re most probably thinking at this stage, “then how do I get my bone quality tested?” And, unfortunately, it’s not that simple.
Although there are methods to measure bone quality that can give a better idea about bone strength and risk of fracture (in comparison to bone density testing), bone quality testing methods are less readily available, invasive, or more expensive than a bone density test. Hence the reason bone density tests are commonly used by doctors over bone quality tests.
Bone density is still an important measurement of bone health. However, we must understand a bone density measurement is only one piece of the puzzle; it is giving you a snapshot of your bone strength at the point in time that test was taken. It is also not telling you if you are losing bone.
You may have a low bone density reading and are not currently losing bone.
Your doctor will require at least two tests over a period of time (and a lab test) to understand if you are losing bone.
HOW OFTEN SHOULD I HAVE MY BONE DENSITY TESTED? - WHEN TO GET YOUR BONES TESTED
If you are a woman over the age of 65 and a man over 70, or if you have any of the risk factors discussed above, it is recommended you get a bone mineral density test.
A follow-up BMD test is recommended at least every two years.
To improve the accuracy of your testing results, make sure you use the exact same machine for each measurement, as different machines may lead to different results.
If you feel you are at risk for osteoporosis or fractures, do not hesitate to speak to your doctor about getting bone density tested.
CAN BONE DENSITY BE IMPROVED OVER 60?
With bone loss and osteoporosis, the best thing that can be done is to prevent it from occurring in the first place. Or preventing further loss in bone mass and strength, and this most certainly can be done.
The question now is, “is it possible to go beyond this and get the bones stronger rather than just preventing them from getting weaker?”
To answer this question, we look back to the components of bone strength that we discussed earlier, that being: bone strength = bone quantity (density) + bone quality.
Studies have shown that when it comes to exercise, exercise programs either show no benefit or only minor benefit when it comes to improving bone mineral density in those with osteoporosis. [11, 12]
On the other hand, however, osteoporosis treatments and exercise have been shown to have beneficial effects on other determinants of bone strength (more specifically bone quality and bone turnover), which can help to strengthen those bones and reduce fracture risk beyond bone mineral density. [13]
By undertaking the right steps, you can improve your bone strength and decrease your risk of fractures.
It’s important now to switch your focus to improving your bone health and being healthy overall.
OSTEOPOROSIS AND MEDICATIONS
I am going to be brief with this section because this is not my area of expertise and something which is best discussed with your doctor.
There are two categories of osteoporosis medications, these being:
Antiresorptive medications - These stop bone loss by suppressing the action of osteoclasts (the cells which break down bone).
Antiresorptive medications include bisphosphonates, denosumab (Prolia), estrogen and hormone therapy, and raloxifene.
Anabolic medications - These increase the rate of bone formation by boosting the activity of osteoblasts (the cells which re-build bone).
The most commonly used anabolic medication for osteoporosis is teriparatide.
Medications do have a place in the treatment of osteoporosis and it will be determined by your doctor if you require them.
The foundation of any bone-strengthening plan, however, should always be nutrition, exercise and other lifestyle factors (which we will cover in part 2).
With everything medical-related that could potentially have long-term effects, it is ok to get a second doctor’s opinion, or even a third if you want to. This way you can hear different perspectives and get a better idea about what is best for you.
Now, let’s get into what you can do to improve your bone health beyond medication.
PART 2: HOW TO EAT FOR STRONGER BONES (AND OTHER FACTORS THAT IMPROVE BONE HEALTH)
SOURCES
CLICK HERE TO VIEW ALL SOURCES USED IN THIS ARTICLE.